New hearing rehabilitation option available
According to the American Hearing Loss Association, approximately 20 percent of people in the U.S. suffer from some form of hearing deficit. The World Health Organization (WHO) estimates that approximately 538 million people worldwide are afflicted with this condition. The WHO also estimates that unaddressed hearing loss imposes a global cost of $750 billion annually as a result of productivity loss as well as health and educational support costs.
There are three basic types of hearing loss. Conductive hearing loss occurs when there is some form of limitation of external sound accessing the structures of the inner ear. Sensorineural hearing loss involves dysfunction at the level of the cochlea (hearing organ) and/ or the hearing nerve itself. Mixed hearing loss is the third classification that occurs when components of sensorineural and conductive hearing loss are both present.
There are many facets to management of patients with irreversible hearing loss. One of the first considerations is to determine if a patient may benefit from instrumentation that can facilitate hearing. An example is a hearing aid which functions to amplify sound for the wearer. Cochlear implantation is considered for those with severe to profound hearing loss of both ears, and it involves surgical placement of an electrode that directly stimulates the hearing organ.
One remarkably effective method of hearing rehabilitation is the bone-anchored hearing device (BAHD) procedure. Historically, the concept of this procedure arose from dental implant experimentation dating back to the mid-1970s. In attempts to test the integrity of bone integration of the implants with sound-producing instruments, it was noted that the subject incidentally perceived sound very clearly. This concept is based on stimulation of the cochlea via direct conduction of signal through bone. Essentially, these systems bypass the external and middle ear and transfer sound energy straight to the fluids of the inner ear. In 1977, the first BAHD prototype was manufactured, and implantation began with great success. By mid-2009, the global number of patients with these devices was estimated to exceed 70,000.
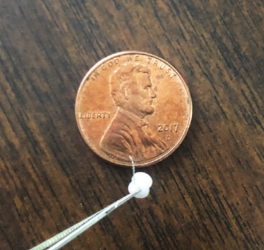
Magnet-based implantable devices are relatively recent developments within the spectrum of BAHD technology. The Sophono implant, developed in Germany in 2006, was approved for use in the United States in May 2011. The device consists of a bi-lobed magnetic titanium implant that is affixed to the skull during a short surgical procedure. One month later, the patient returns for placement of the external component of the device, which consists of a sound processor and a magnetic baseplate. Essentially, the sound processor is held in place by the baseplate, which, in turn, is held to the skin by the implanted titanium magnet. The processor is thus able to transmit vibrations through skin to bone and ultimately to the inner ear.
There are many applications of BAHD technology for hearing rehabilitation. Patients who have irreversible conductive hearing loss can benefit from this procedure because the bone-anchored system completely bypasses the site causing the conductive loss (i.e., the outer and middle ear). Patients with mixed hearing loss may also benefit from the procedure. Another indication is for patients who suffer from single-sided deafness. In this situation, the implant may be placed on the side of the deaf ear. Sound is then transmitted via bone to the side of the good ear such that the patient essentially “hears” from both sides through one good ear. The Sophono implant is approved for ages 5 years and older.
I had the privilege of performing the first-ever Sophono implant procedure in the Shreveport-Bossier City area inSeptember 2016 on a patient who suffered from a sudden hearing loss in one ear that could not be helped with a traditional hearing aid. Since then, we have had continued success with subsequent patients, as well.
Magnetic-based implantable device technology can provide a very effective means of hearing rehabilitation. This is an exciting tool in our armamentarium as ENT specialists, and it is now available in the Shreveport-Bossier City area.
Dr. Chuka Ifeanyi is an ear, nose & throat specialist at Highland Clinic. Dr. Ifeanyi specializes in the diagnosis and treatment of disorders affecting the ear, nose, throat, and the head and neck of both children and adults. He is accepting new patients and can be reached at 798-4440; located at 1455 East Bert Kouns Industrial Loop, Suite 206, Shreveport, LA 71105.